TB Elimination by 2030: Are We on Track?
- Caroline Van Cauwelaert
- Mar 24
- 3 min read
March 24 marks World TB Day – a global call to accelerate efforts toward ending TB. In 2014, the World Health Organization (WHO) launched the End TB Strategy, setting an ambitious target: a 90% reduction in TB deaths and an 80% reduction in new TB cases by 2030, compared to 2015 levels. With just a few years remaining, it’s time to assess our progress. Are we truly on track to eliminate TB by 2030?
Progress so far
Since 1997, WHO has published an annual global TB report to monitor the epidemic. The 2024 report highlighted both progress and persistent challenges:
The surge in TB cases triggered by COVID-19 has slowed and stabilised.
Global TB cases: While still higher than pre-pandemic levels – 10.8 million in 2023 compared to 10.7 million in 2022 – much of this increase is due to population growth rather than a worsening outbreak.
TB incidence rate: 134 per 100,000 people, showing only a minor 0.2% increase from 2022.
TB deaths: Declined from 1.32 million in 2022 to 1.25 million in 2023, continuing the post-COVID downward trend.
These improvements are largely due to the recovery of TB diagnosis and treatment services after pandemic-related disruptions. However, progress remains slow, and key milestones remain unmet.
Challenges and gaps
Despite progress, TB remains the leading infectious cause of death worldwide, surpassing COVID-19. More worryingly, we are far from achieving the 2025 milestones:
Reduction in TB incidence since 2015: Only 8.3% – this is far behind the 50% reduction goal by 2025.
Reduction in TB deaths since 2015: Only 23%, compared to the 75% goal by 2025.

Source: Global tuberculosis report 2024
The numbers make it clear: without urgent action, we will not meet the 2030 targets.
Barriers preventing progress
Several critical barriers continue to hinder global efforts to eliminate TB:
Insufficient Funding: In 2023, only $5.7 billion was allocated for TB services – falling far short of the $13 billion target set by WHO member states. Recent U.S. funding cuts to global TB programs have further strained resources. USAID, one of the largest funders of international TB efforts, slashed its TB budget, impacting treatment, research, and frontline healthcare. This has put 18 of the highest-burden countries at significant risk. Last year alone, US aid helped avert 3.65 million deaths.
Drug Resistance: Multidrug-resistant Tuberculosis (MDR-TB) and extensively drug-resistant TB (XDR-TB) make treatment more complex, requiring longer, costlier regimens.
Healthcare Disruptions: The COVID-19 pandemic significantly impacted TB services, delaying diagnoses and treatment for millions.
Social Determinants of HealthPoverty, malnutrition, and limited healthcare access continue to fuel TB transmission, particularly in high-burden regions. Locating vulnerable populations is vital.
Stigma and Misinformation: Fear and misinformation prevent many from seeking timely TB care, leading to delayed diagnosis and further spread of the disease.
A path forward
There is no denying that recent USAID cutbacks will have devastating consequences for low- and middle-income countries, exacerbating conditions on the ground and leading to immense human suffering. However, emerging advancements –such as more effective treatment regimens and AI-powered tools for enhanced diagnosis and hotspot tracking – offer a glimmer of hope in the fight against TB.
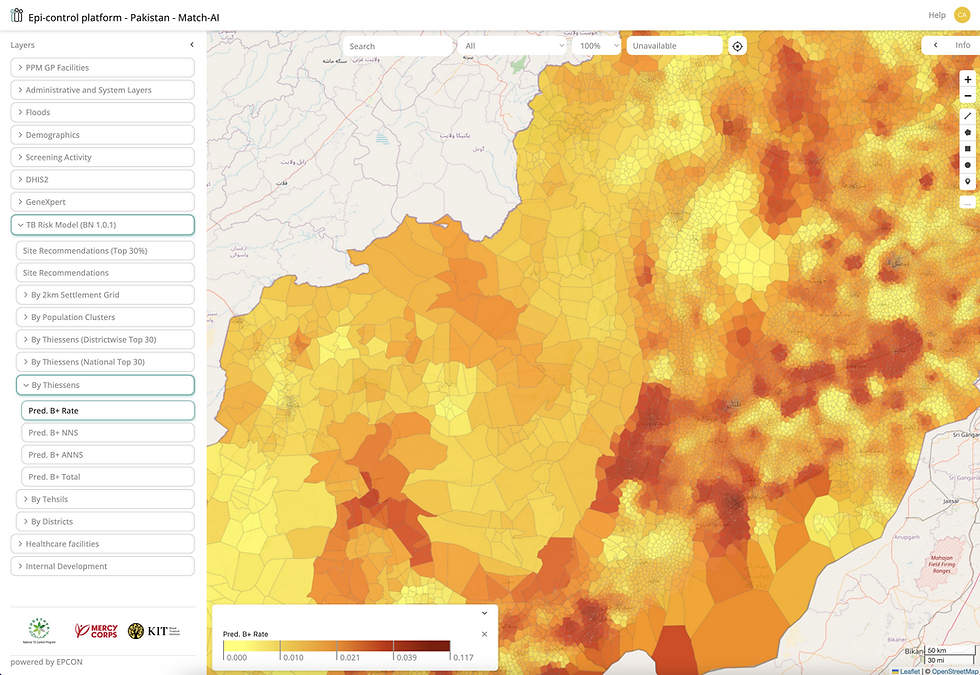
Our technology, the Epi-control platform for infectious disease management is designed to improve efficiency and expand access to critical care.